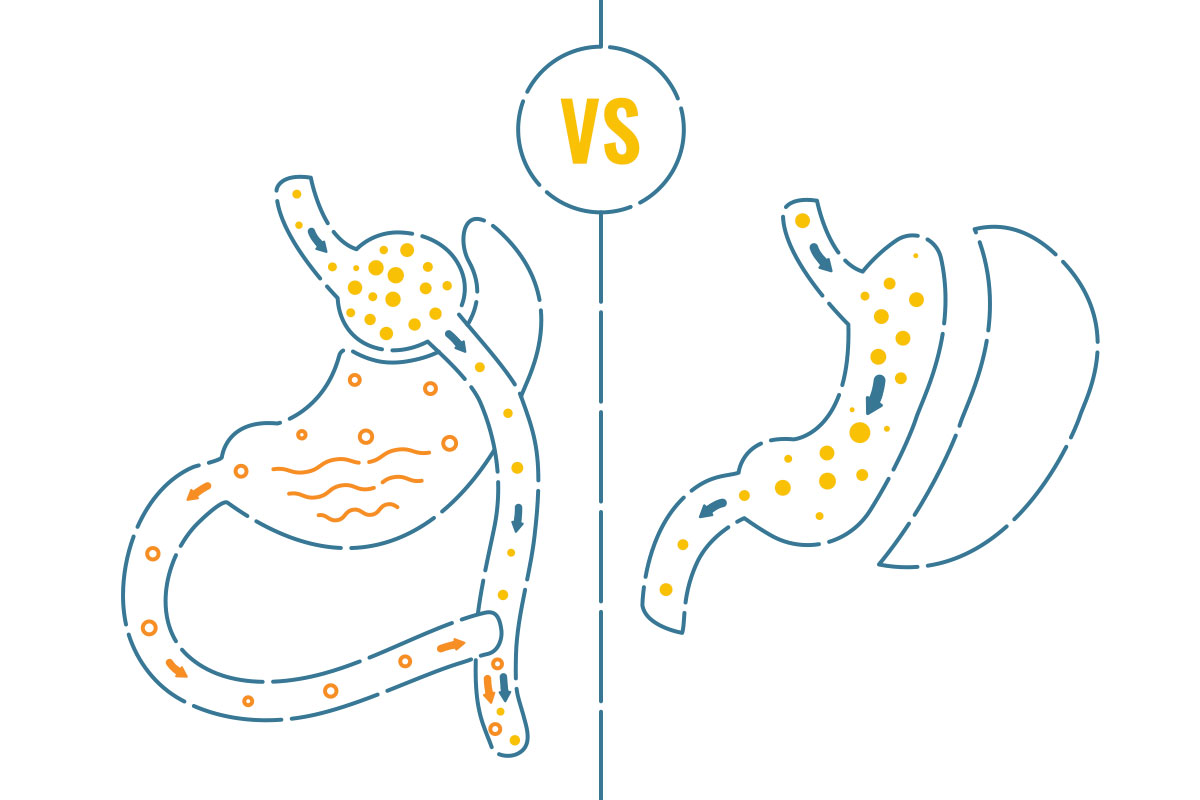
The sleeve gastrectomy and the gastric bypass are considered to be two of the safest and most effective surgical procedures for weight loss. The gastric bypass treatment involves rerouting the small intestine to a small stomach pouch, while the gastric sleeve procedure involves removing a section of the stomach to construct a smaller stomach in the shape of a sleeve. Both procedures have the potential to result in significant weight loss and an improvement in the health problems that are associated with obesity.
It’s essential to have a solid understanding of the benefits offered by both options so you can make an educated choice on which one would be best suited for your particular situation.
5 Advantages of Sleeve Gastrectomy Over Gastric Bypass
Sleeve Gastrectomy is Less Invasive than Gastric Bypass
Patients often ask me if the sleeve is “less invasive” than the bypass. I certainly understand the spirit of the question, but I tend to think of the bypass as a more “aggressive” procedure than an “invasive” one.
Both the sleeve gastrectomy and the gastric bypass…
- …can be performed laparoscopically.
- …enter the abdominal cavity.
- …result in nearly identical hospital stays and short-term lifting restrictions.
- …require similar methods of advancing dietary intake from clear thin liquids to a bariatric regular diet over 6 to 8 weeks after surgery.
The difference between the two is that the bypass requires disconnecting and reconnecting the small bowel. This results in better outcomes for the bypass, but also slightly increases complication rates. In that sense, the sleeve is less “invasive”—or, put into terms that I like a little more, the bypass is a little more “aggressive.”
Sleeve Gastrectomy Has Shorter Operative Times than Gastric Bypass
The reason the operative time of a surgery matters is related to anesthesia. When the anesthetic time is cut down, the patient has a lower risk of complications such as deep venous thrombosis and pulmonary issues.
The operative time for a sleeve gastrectomy is around 30 minutes, while the gastric bypass is usually around 90 minutes. Of course, these are average times and many things can prolong the surgical time of a procedure. Regardless, the sleeve is, on average, a less time-consuming operation. This is primarily due to the fact that the gastric sleeve is a less complex treatment: it just involves the shrinking of the stomach, not the rerouting of the small intestine.
Sleeve Gastrectomy Has a Lower Overall Risk of Complications than Gastric Bypass
As a less complex procedure that involves less operative time, it stands to reason that the sleeve gastrectomy has a lower overall complication rate than the gastric bypass.
A large study looked at over 130,000 patients from the 2015 Metabolic and Bariatric Surgery Accreditation and Quality Improvement (MBSAQIP) data registry. The study documented that the sleeve had approximately “half the risk-adjusted odds of death, serious morbidity, and leak within the first 30 days” when compared to the bypass.
The bypass, which is about as safe as gallbladder surgery, is very safe; the sleeve is safer still. A surgeon may encourage the sleeve instead of the bypass due to the higher risk of a particular patient.
Sleeve Gastrectomy Does Not Reroute the Intestines
During a sleeve gastrectomy, the stomach is reshaped into roughly the size and shape of a banana. Since the body’s natural digestive process is not disrupted, this reduces (but doesn’t eliminate) the risk of complications such as dumping syndrome and malnutrition.
The act of rerouting the intestines introduces a potential long-term complication to the gastric bypass surgery: an internal hernia, which one article defines as “the protrusion of abdominal viscera, most commonly small bowel loops, through a peritoneal or mesenteric aperture into a compartment in the abdominal or pelvic cavity.”
Now that that’s perfectly clear, I’ll restate that definition. In the context of a gastric bypass, an internal hernia is the sliding of the intestines through a hole created by the procedure. This can cut off the blood flow to the bowel, causing it to die.
Most papers quote the incidence of internal hernia at around 1% to 5%, making it an uncommon problem. However, the fact remains that it is a problem that is created by the new anatomy of the bypass. The absence or decreased risk of these complications makes the sleeve gastrectomy a more attractive option for some patients.
Sleeve Gastrectomy Has a Lower Risk of Malnutrition & Vitamin Deficiencies than Gastric Bypass
Gastric bypass surgery can have a higher rate of vitamin and nutritional deficiencies due to the rerouting of the small intestine. Since there is no small bowel manipulation with the sleeve, the risk of protein and micronutrient deficiencies are less common. Since there is a risk with either procedure, it’s important to have preoperative nutritional counseling, vitamin supplementation, and lifelong monitoring and nutritional reinforcement.
5 Advantages of Gastric Bypass Over Sleeve Gastrectomy
Gastric Bypass Typically Results in Greater Weight Loss than Sleeve Gastrectomy
The gastric bypass procedure not only reduces the size of the stomach, but also reroutes the small intestine. This alters the method by which the body absorbs food, which in turn reduces the number of calories absorbed. As a result, patients who have a gastric bypass typically experience a more dramatic and rapid weight loss, with most patients losing between 70% and 80% of their excess weight within the first five years after surgery.
On the other hand, the sleeve gastrectomy procedure only reduces the size of the stomach. This can lead to substantial weight loss, with the average patient losing between 60% and 70% of their excess body weight.
While both procedures can be effective in helping patients achieve a healthy weight, the gastric bypass offers a greater potential for weight loss and is often recommended for patients who have a higher body mass index (BMI).
Weight Loss with Gastric Bypass is More Sustainable & Longer-Lasting than Weight Loss with Sleeve Gastrectomy
Studies have shown that the overwhelming majority of patients who have undergone gastric bypass are able to maintain a significant percentage of their weight loss over the long term. The sleeve gastrectomy can also lead to outstanding weight loss, and while it’s effective over the long term as well, it’s not as effective when compared to the gastric bypass.
Interestingly, it’s difficult to nail down exact numbers since there’s no universally agreed-upon definition of what weight regain looks like. Is it gaining any weight? Is it gaining 10% of your weight back? Is it gaining back 50% or 100% of what you lost?
Come to think of it, no one really agrees on what “long term” means, either. Is it one year? Is it five years? Is it a decade? Is it the remainder of the life of the patient?
Regardless, most surgeons would agree that while both procedures can be effective tools in helping patients achieve a healthy weight and maintain that weight loss over time, the gastric bypass offers a more durable solution for most patients.
Gastric Bypass is a Better Treatment for Diabetes than Sleeve Gastrectomy
It’s been shown over and over again in the literature: type 2 diabetes responds remarkably well to the metabolic changes of the gastric bypass. It’s also true that diabetes responds to sleeve gastrectomy, but when placed head-to-head, the bypass is the clear winner when it comes to addressing the medical needs of the diabetic.
While it’s hard to pick one single article to highlight, a study in the Annals of Surgery documented that 92% of diabetics were either improved or cured with a bypass, while 83% of diabetics were either improved or cured with a sleeve gastrectomy. Either way, the results for the benefits of bariatric surgery for the diabetic are so overwhelming that the American Diabetes Association has stated that obese diabetics who fail weight loss or improvements in comorbidities should all be recommended for surgical evaluation.
Overall, both procedures are excellent for the resolution of diabetes, but the gastric bypass offers a better solution.
Gastric Bypass is a Better Treatment for Gastroesophageal Reflux Disease (GERD) than Sleeve Gastrectomy
The pouch created by a gastric bypass is very small—in fact, it’s around an ounce in size. The remainder of the acid-secreting portions of the stomach is isolated from the esophagus. The diversion of the intestines also effectively prevents bile from refluxing, which is another concern.
Additionally, it has been shown that one of the common causes of reflux is the increased intra-abdominal pressure associated with obesity. The bypass addresses the root cause of GERD by causing weight loss and thus decreasing intra-abdominal pressure.
When you look at the literature, GERD is objectively resolved or improved in 92% of patients after the gastric bypass; conversely, most studies indicate that around 15% to 20% of patients have significant GERD after sleeve gastrectomy.
Gastric Bypass Has a Longer Track Record than Sleeve Gastrectomy
The gastric bypass as we know it was first conceived and performed by Dr. Edward Mason at the University of Iowa in 1966. Since that time, millions of gastric bypasses have been performed, and thousands upon thousands of articles have been published. As a result, the gastric bypass is considered a well-established procedure with a proven track record of success.
On the other hand, the sleeve gastrectomy is a relatively new procedure, with the first sleeve being performed in 1999. The sleeve gastrectomy has also been extensively studied and is currently the most common bariatric procedure worldwide, but it still has a shorter track record when compared to the gastric bypass.
How to Choose Between Sleeve Gastrectomy and Gastric Bypass
In my own practice, there are a few things that go into a recommendation for a bypass versus a sleeve for any patient. For example:
- Patient choice is, of course, paramount. Most people qualify for both procedures, so if they have a strong opinion, that can usually be accommodated.
- If a patient has severe GERD or diabetes, I try to lean them toward a gastric bypass.
- If a patient’s BMI is high, I tend to have them consider the bypass a little more strongly due to the slightly increased and more sustainable weight loss associated with the procedure.
Additionally, there are individual concerns, previous diagnoses, and medications that would force us down one pathway or another. Because of this, it’s crucial to have a full discussion concerning your particular situation. By taking the time to discuss the options with your bariatric surgeon, you can make a confident and informed decision about which procedure is right for you.
Regardless of whether you choose a gastric sleeve or a gastric bypass, both procedures require a significant commitment to long-term lifestyle changes in order to achieve optimal success. Maintaining and improving your health requires making substantial dietary modifications and embracing an active lifestyle, including regular exercise. It’s important to keep in mind that neither procedure can provide a long-term solution on its own, and sustained effort on your part is necessary for maximum results. By making these necessary changes to your diet and lifestyle, you can ensure that you are able to maintain your weight loss and enhance your overall health.
Talk to a Bariatric Surgeon About Sleeve Gastrectomy vs. Gastric Bypass
The gastric sleeve procedure can be a highly effective way for those struggling with obesity to lose weight and improve their overall health. With its many benefits, including a high level of safety, shorter operative times, low risk of nutritional deficits, and outstanding outcomes, sleeve gastrectomy is an option that’s worth considering for anyone looking to make a positive change in their life.
Likewise, the gastric bypass is a fantastic choice for many patients. It has a large number of potential benefits, including superior weight loss, low recidivism, and higher cure or improvement rates in diabetics and those suffering from GERD.
Only a conversation with your bariatric surgeon will equip you to make the best decision in your individual situation. If you have not had an initial consultation with a bariatric surgeon, my partners and I would be honored to accept you as a patient at Arkansas Heart Hospital’s Bariatric & Metabolic Institute, located right outside of Little Rock in Bryant.
